Ever wondered how the world tackles the growing challenge of obesity? It’s not just about individual choices; it’s a complex web of societal factors, medical interventions, and policy decisions. From the pharmaceutical industry’s role to the impact of socioeconomic disparities, understanding obesity health policy is key to finding effective solutions. This exploration delves into the multifaceted landscape of obesity, examining its causes, consequences, and the strategies implemented – and needed – to combat this global health crisis.
We’ll journey through the various approaches to obesity management, from government policies and pharmaceutical interventions to technological advancements and community-based initiatives. We’ll also explore the ethical considerations surrounding treatment options and the critical role played by healthcare professionals. Get ready for an engaging deep dive into a topic that affects us all!
Defining Obesity and its Health Impacts
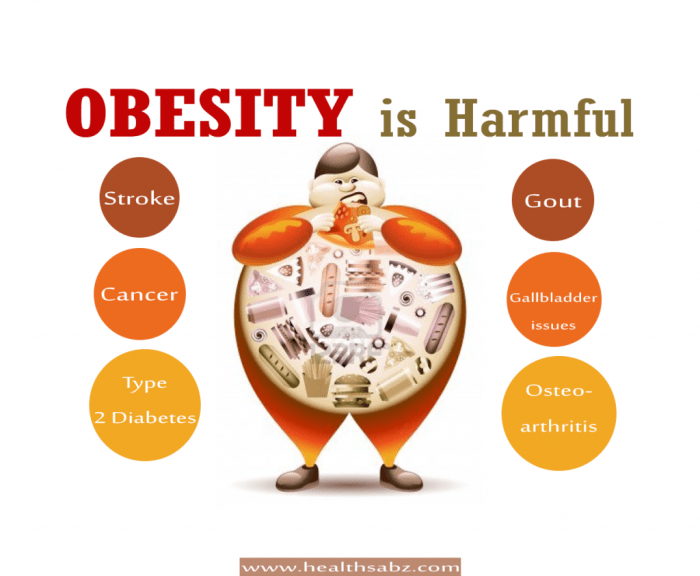
Obesity is a significant global health concern, characterized by an excessive accumulation of body fat that presents a risk to health. It’s not simply about aesthetics; it’s a complex condition with far-reaching consequences for individual well-being and societal resources. Understanding its various classifications and health impacts is crucial for effective prevention and treatment strategies.
Obesity Classifications and Associated Health Risks
Obesity is typically classified using the body mass index (BMI), calculated as weight in kilograms divided by the square of height in meters (kg/m²). While BMI isn’t a perfect measure, it provides a useful screening tool. Classifications generally include overweight (BMI 25-29.9 kg/m²) and obesity (BMI ≥ 30 kg/m²), further subdivided into Class I (30-34.9 kg/m²), Class II (35-39.9 kg/m²), and Class III (≥ 40 kg/m²), also known as severe or morbid obesity.
Higher BMI classifications are associated with a progressively increased risk of numerous health problems. For instance, individuals with Class III obesity face a significantly higher likelihood of developing type 2 diabetes, heart disease, and certain types of cancer compared to those with Class I obesity or those who are merely overweight.
Long-Term Consequences of Obesity on Major Organ Systems
Obesity places a considerable strain on multiple organ systems.
Cardiovascular System Impacts
Excess weight increases the workload on the heart, leading to hypertension (high blood pressure), hyperlipidemia (high cholesterol), and an increased risk of coronary artery disease, heart failure, and stroke. The added stress on the cardiovascular system can manifest as shortness of breath, chest pain, and irregular heartbeats. For example, a study published in the
Lancet* demonstrated a strong correlation between high BMI and increased risk of cardiovascular events.
Respiratory System Impacts
Obesity can lead to obstructive sleep apnea (OSA), a condition where breathing repeatedly stops and starts during sleep. This can result in daytime sleepiness, fatigue, and decreased cognitive function. Furthermore, excess abdominal fat can restrict lung expansion, leading to reduced lung capacity and increased shortness of breath, even during mild exertion. The increased risk of respiratory infections is also notable.
Endocrine System Impacts
Obesity significantly impacts the endocrine system, often leading to insulin resistance and type 2 diabetes. Excess fat tissue produces hormones and inflammatory substances that interfere with insulin’s ability to regulate blood sugar levels. This can lead to hyperglycemia (high blood sugar), increasing the risk of long-term complications such as kidney disease, nerve damage, and blindness. Polycystic ovary syndrome (PCOS) is another endocrine disorder frequently associated with obesity in women.
Societal Burden of Obesity
The societal impact of obesity is substantial, encompassing significant economic and social costs.
Economic Implications
Obesity contributes to increased healthcare expenditures due to higher rates of chronic diseases and their associated treatments. Lost productivity from absenteeism and reduced work capacity also adds to the economic burden. The costs associated with obesity-related complications, such as diabetes management and cardiovascular surgeries, place a considerable strain on healthcare systems worldwide. For instance, the Centers for Disease Control and Prevention (CDC) estimates billions of dollars are spent annually in the United States on obesity-related healthcare costs.
Social Implications
Obesity can lead to social stigma and discrimination, affecting individuals’ self-esteem, mental health, and social interactions. This can result in social isolation and decreased quality of life. Furthermore, obesity is often associated with reduced participation in physical activities and social events, further exacerbating its negative social consequences. The societal perception of obesity contributes to a complex interplay of factors impacting individuals’ well-being and societal integration.
Current Obesity Health Policies and Interventions

The global fight against obesity requires a multifaceted approach, encompassing policy changes, public health interventions, and individual behavioral modifications. Different countries have adopted diverse strategies, reflecting their unique socio-economic contexts and healthcare systems. Examining these policies and their effectiveness provides valuable insights for developing more impactful interventions.
A comparative analysis reveals a wide spectrum of approaches. Some countries, like Mexico, have implemented significant taxes on sugary drinks, resulting in demonstrable reductions in consumption. Others, such as the United Kingdom, have focused on promoting healthier food choices through public awareness campaigns and nutritional labeling regulations. Meanwhile, countries in Scandinavia often emphasize community-based interventions, incorporating physical activity into daily life through urban planning and school programs.
The success of these varied approaches highlights the importance of tailoring interventions to specific cultural and environmental factors.
Successful Obesity Prevention and Management Strategies
Several strategies have demonstrated effectiveness in preventing and managing obesity globally. These include comprehensive school-based programs that integrate nutrition education, physical activity, and behavior modification techniques. Furthermore, community-based initiatives that promote access to healthy food options, create safe spaces for physical activity, and foster supportive social environments have yielded positive results. National-level policies such as taxes on unhealthy foods and subsidies for fruits and vegetables can also significantly influence dietary choices.
Finally, integrated healthcare approaches that incorporate obesity management into routine primary care have proven beneficial in addressing individual needs.
Limitations and Challenges of Existing Obesity Policies
Despite considerable efforts, many challenges hinder the effectiveness of current obesity policies. One major hurdle is the complexity of obesity, which is influenced by a multitude of factors including genetics, environment, and socioeconomic status. Furthermore, the implementation of policies often faces political and economic obstacles, with powerful lobbying groups from the food and beverage industry sometimes hindering progress.
Measuring the long-term impact of interventions can also be challenging, requiring robust data collection and analysis over extended periods. Finally, the lack of consistent data collection and evaluation across different countries makes it difficult to compare the effectiveness of various strategies and learn from best practices.
Comparative Analysis of Obesity Interventions
The following table provides a comparative analysis of the effectiveness of four different interventions:
| Intervention Type | Target Population | Implementation Method | Outcomes |
|---|---|---|---|
| Sugar-Sweetened Beverage Tax | General Population | Tax levied on sugary drinks | Reduced consumption of sugary drinks; mixed evidence on overall weight reduction. Effectiveness varies depending on tax level and complementary interventions. Example: Mexico’s tax led to a decrease in sugary drink purchases, but impact on overall obesity rates is still under evaluation. |
| School-Based Nutrition and Physical Activity Programs | Children and Adolescents | Curriculum integration, school-based interventions, and changes to school environments | Improved knowledge and attitudes toward healthy eating and physical activity; modest improvements in BMI and fitness levels; long-term effects require further investigation. Example: Many school-based programs show short-term success but struggle with sustained impact after program completion. |
| Community-Based Interventions | Local Communities | Creation of supportive environments for healthy eating and physical activity, community gardens, and safe recreational spaces | Improved access to healthy food options; increased physical activity levels; positive social and environmental changes. Example: Studies have shown improvements in community health metrics in areas with enhanced access to green spaces and healthy food options. |
| National Public Awareness Campaigns | General Population | Television, radio, and online advertising campaigns promoting healthy lifestyles | Increased awareness of healthy eating and physical activity; limited impact on long-term behavior change unless coupled with other interventions. Example: While public awareness campaigns can increase knowledge, sustained behavioral changes often require more comprehensive strategies. |
Role of the Pharmaceutical Industry in Obesity Management
The pharmaceutical industry plays a significant, albeit controversial, role in the management of obesity. While offering potential solutions for individuals struggling with weight loss, the use of pharmaceutical interventions raises complex ethical considerations and necessitates careful consideration of potential side effects. Understanding the various approaches, their implications, and the need for responsible use is crucial for effective obesity management strategies.
Pharmaceutical approaches to obesity treatment primarily focus on altering the body’s metabolic processes to reduce appetite, limit fat absorption, or increase energy expenditure. These approaches are often used in conjunction with lifestyle modifications such as diet and exercise, and are generally recommended only for individuals with a BMI exceeding a certain threshold, or those with obesity-related comorbidities.
Pharmaceutical Approaches to Obesity Treatment
Several classes of drugs target different aspects of energy balance and body weight regulation. These medications are not a quick fix and require careful monitoring by healthcare professionals.
Appetite suppressants, for example, work by affecting neurotransmitters in the brain that regulate hunger and satiety. These medications can reduce feelings of hunger, leading to decreased food intake. Examples include phentermine and lorcaserin. Lipase inhibitors, on the other hand, work by blocking the absorption of dietary fat in the intestines. Orlistat is a commonly used lipase inhibitor.
Finally, some medications, such as semaglutide and liraglutide, work by mimicking the effects of incretin hormones, which regulate glucose homeostasis and appetite.
Ethical Considerations and Potential Side Effects
The use of pharmaceutical interventions for obesity is not without ethical considerations. Concerns exist regarding potential side effects, the long-term efficacy of these medications, and the potential for misuse or over-reliance on medication as a primary weight management strategy, rather than a component of a holistic approach.
Side effects can vary depending on the specific medication but may include nausea, constipation, diarrhea, dizziness, headache, and increased blood pressure or heart rate. Some medications may also interact with other medications, highlighting the need for careful medical supervision. Furthermore, the long-term effects of many of these drugs are not fully understood, and the possibility of dependence or withdrawal symptoms needs to be carefully considered.
The potential for these medications to be misused or to create an unrealistic expectation of weight loss without lifestyle changes is also a significant concern.
Public Awareness Campaign: Responsible Medication Use in Obesity Management
A comprehensive public awareness campaign is needed to promote responsible medication use in obesity management.
Target Audience: Individuals with obesity and their healthcare providers, as well as the general public. Specific messaging should be tailored to each group.
Messaging: The campaign should emphasize that medication is only one component of a holistic approach to weight management. It should highlight the importance of lifestyle changes, including diet and exercise, as essential elements of successful weight loss and long-term maintenance. The campaign should also accurately portray the potential benefits and risks of various medications, emphasizing the importance of consulting with a healthcare professional to determine the most appropriate treatment plan.
The campaign should strongly discourage self-medication and emphasize the need for careful monitoring and adherence to prescribed dosages and treatment plans.
Media Channels: A multi-pronged approach utilizing various media channels would be most effective. This could include television and radio advertisements, social media campaigns, print media (newspapers, magazines), and partnerships with healthcare organizations and community groups. Educational materials, such as brochures and online resources, should also be developed to provide detailed information about the responsible use of medication in obesity management.
The Pharmacy’s Role in Obesity Prevention and Treatment
Pharmacies, traditionally viewed as dispensing centers, are increasingly recognized as crucial players in the fight against obesity. Their accessibility, coupled with pharmacists’ expertise in medication management and patient interaction, positions them uniquely to contribute to both prevention and treatment efforts. This section will explore how pharmacies can actively participate in combating this widespread health concern.Pharmacists’ Expertise in Patient Education and Counseling on Obesity ManagementPharmacists possess the knowledge and skills to provide crucial patient education and counseling regarding obesity management.
This includes explaining the risks associated with obesity, discussing lifestyle modifications like diet and exercise, and helping patients understand and manage their medications, including any potential side effects that might contribute to weight gain or hinder weight loss. Beyond medication-specific advice, pharmacists can also offer guidance on over-the-counter products and supplements related to weight management, emphasizing the importance of informed choices and responsible use.
They can empower patients to make informed decisions about their health, fostering a collaborative approach to weight management.
Pharmacy Contributions to Community-Based Obesity Prevention Programs
Pharmacies can serve as vital community hubs for obesity prevention programs. Their accessibility and established relationships with local residents make them ideal locations for initiatives aimed at promoting healthy lifestyles. Pharmacies can participate in community health fairs, offering weight management information and screenings. They can partner with local organizations to deliver educational programs on nutrition, physical activity, and healthy eating habits.
Pharmacists can also play a key role in distributing educational materials and promoting community resources related to weight management. This proactive community engagement is crucial in shifting community-wide health behaviors.
Examples of Successful Pharmacy-Based Interventions
Several successful pharmacy-based interventions demonstrate the positive impact of pharmacist involvement in obesity management.
- Weight Management Programs Integrated into Pharmacy Services: Many pharmacies have implemented structured weight management programs. These programs typically involve initial assessments, personalized counseling sessions with pharmacists, regular monitoring of weight and other health indicators, and ongoing support. One example is a program where pharmacists provided individualized counseling, focusing on dietary changes, physical activity, and behavior modification. This resulted in significant weight loss and improvements in other health markers among participants compared to a control group.
The program’s success highlighted the effectiveness of personalized care delivered in an accessible setting.
- Medication Therapy Management (MTM) for Obesity-Related Medications: Pharmacists can play a vital role in MTM for patients taking medications that can affect weight. This includes reviewing medication lists, identifying potential drug interactions, and educating patients on how to manage side effects. For example, a study demonstrated that MTM services significantly improved medication adherence and patient understanding of their medications, leading to better weight management outcomes for patients using anti-diabetic medications, which often lead to weight gain.
- Community Outreach and Educational Initiatives: Pharmacies can actively participate in community-based initiatives to raise awareness about obesity and promote healthy lifestyles. This can include hosting health fairs, providing educational materials, and collaborating with local organizations to deliver health promotion programs. One example is a pharmacy chain that partnered with local schools to implement a nutrition education program, leading to improved dietary habits among students and a reduction in childhood obesity rates in the community.
The partnership created a lasting impact on the community’s health.
Addressing Socioeconomic Factors in Obesity
Obesity doesn’t affect everyone equally. A significant body of research demonstrates a strong correlation between socioeconomic status (SES) and the prevalence of obesity, revealing a complex interplay of factors that disproportionately impact lower-income communities. Understanding this relationship is crucial for developing effective and equitable public health interventions.The relationship between socioeconomic status and obesity prevalence is multifaceted. Lower SES is often associated with increased exposure to obesogenic environments, characterized by limited access to healthy, affordable food options, lack of safe spaces for physical activity, and higher stress levels.
Conversely, higher SES individuals often have greater resources to afford nutritious food, participate in recreational activities, and access healthcare services for weight management. This disparity contributes to a widening health gap, with those in lower socioeconomic brackets experiencing a higher burden of obesity-related diseases.
Food Insecurity and Access to Healthy Food
Food insecurity, the state of being without reliable access to a sufficient quantity of affordable, nutritious food, is a major driver of obesity, particularly among low-income families. Families struggling to make ends meet often rely on cheaper, calorie-dense processed foods, high in sugar, fat, and sodium, which are readily available but lack essential nutrients. These foods contribute to weight gain and increase the risk of developing chronic diseases.
Simultaneously, access to fresh produce, whole grains, and other healthy foods is often limited in low-income neighborhoods, creating what’s known as a “food desert.” These areas often lack supermarkets and grocery stores, leaving residents reliant on convenience stores and fast-food restaurants, which typically offer limited healthy choices. This lack of access to nutritious food options exacerbates the challenges faced by individuals striving to maintain a healthy weight.
For example, a study conducted in South Central Los Angeles showed a significant correlation between the density of fast-food restaurants and the prevalence of obesity in the surrounding communities.
Policy Proposal: Community-Based Nutrition and Fitness Initiative
To address the socioeconomic determinants of obesity within a specific community – let’s consider a hypothetical urban neighborhood with high rates of food insecurity and limited access to recreational facilities – a comprehensive, multi-pronged approach is needed. This initiative, termed the “Community Thrive Program,” would focus on improving access to healthy food and promoting physical activity through several key strategies.First, the program would establish a community garden, providing residents with the opportunity to grow their own fruits and vegetables.
This would not only increase access to fresh produce but also foster a sense of community and provide educational opportunities about healthy eating. Secondly, the program would partner with local grocery stores to offer discounts on healthy food items for low-income residents, potentially through a voucher system. This would make nutritious options more affordable and accessible. Thirdly, the program would work to create safe and accessible spaces for physical activity, such as renovating existing parks or creating walking trails.
This would encourage physical activity and provide opportunities for social interaction. Finally, the program would offer cooking classes and nutrition education workshops to empower residents with the knowledge and skills to make healthier food choices. This educational component is crucial for long-term behavior change and sustainable improvements in health outcomes. The program would be evaluated using a combination of quantitative and qualitative methods to assess its impact on obesity rates, food security, and community well-being.
Data collected would include changes in BMI, self-reported dietary habits, and participation rates in program activities. Qualitative data would be gathered through focus groups and interviews to capture the perspectives and experiences of program participants. This data-driven approach would allow for ongoing program refinement and adaptation to maximize its effectiveness.
Technological Interventions in Obesity Management
The fight against obesity is increasingly leveraging the power of technology. Wearable devices, mobile applications, and sophisticated digital platforms are transforming how we monitor weight, track dietary intake, and promote healthier lifestyles. These tools offer personalized feedback, increased accountability, and opportunities for engagement that were previously unavailable. This section explores the diverse landscape of technological interventions and their impact on obesity management.
Technological interventions offer a multifaceted approach to obesity management, encompassing various tools and strategies designed to improve patient engagement and promote sustainable lifestyle changes. These interventions are not merely technological advancements; they represent a shift towards personalized, data-driven approaches to healthcare, addressing the complex interplay of behavioral, environmental, and physiological factors contributing to obesity.
Effectiveness of Wearable Devices and Mobile Apps in Weight Management
Wearable devices, such as smartwatches and fitness trackers, provide continuous monitoring of physical activity, sleep patterns, and sometimes even heart rate variability. Mobile applications often complement these devices, offering features like calorie tracking, personalized meal planning, and progress visualization. Studies have shown varying degrees of effectiveness, with some demonstrating significant weight loss in users who actively engage with the technology.
However, the success of these interventions is highly dependent on user adherence and motivation. For example, a study published in the Journal of the American Medical Association found that individuals using wearable fitness trackers experienced a modest but statistically significant increase in physical activity compared to a control group. However, another study highlighted that the long-term effectiveness of these devices diminishes if users lose motivation or fail to integrate the data into their lifestyle changes.
Comparison of Different Technological Interventions
Different technological interventions vary significantly in their features, functionality, and effectiveness. While some focus primarily on activity tracking, others incorporate more comprehensive features, including dietary monitoring, social support networks, and gamified challenges. For instance, apps focusing on cognitive behavioral therapy (CBT) techniques often show greater success in long-term weight management compared to simple calorie counters. The effectiveness also depends on the user’s specific needs and preferences.
A person who enjoys competitive challenges might find a gamified app more motivating than a simple activity tracker. Conversely, someone who prefers a more structured approach might benefit from an app that integrates with a registered dietitian or personal trainer.
Visual Representation of Technology’s Role in Enhancing Patient Engagement
Imagine a dynamic dashboard on a patient’s smartphone. The central display shows a clear, easily understandable graph charting their weight loss progress over time. Around this central graph are smaller, interactive modules. One module displays a colorful pie chart showing their daily macronutrient intake, with customizable targets for each nutrient. Another module presents a calendar view, highlighting days with high activity levels and providing positive reinforcement through visual cues.
A fourth module shows a leaderboard, showcasing the patient’s ranking among their support group within the app (optional, emphasizing the social aspect). Finally, a button connects the patient directly to a virtual appointment with their healthcare provider, facilitating seamless communication and support. This integrated, visual representation fosters continuous monitoring, provides personalized feedback, and promotes sustained engagement throughout the weight management journey.
The interactive elements, such as the customizable targets and the social leaderboard, create a sense of ownership and accountability, thereby increasing adherence to the treatment plan.
Future Directions in Obesity Health Policy
The fight against obesity requires a multifaceted approach that evolves with our understanding of the condition and its complex interplay with societal factors. Future obesity health policies must adapt to emerging trends, embrace innovative strategies, and prioritize research to effectively tackle this global health challenge. Success will depend on a collaborative effort between policymakers, healthcare professionals, researchers, and individuals themselves.
The effectiveness of future policies hinges on a dynamic approach that accounts for shifting demographics, technological advancements, and a deeper understanding of the biological and environmental drivers of obesity. This requires a shift from reactive measures to proactive strategies that focus on prevention and early intervention, rather than solely managing the consequences of obesity.
Personalized Obesity Management Strategies
Personalized medicine is transforming healthcare, and obesity management is no exception. Future policies should incentivize the development and implementation of personalized interventions tailored to an individual’s genetic predisposition, lifestyle, environment, and cultural context. This could involve genetic testing to identify individuals at higher risk, followed by targeted lifestyle modifications or pharmacological interventions. For example, a policy could offer subsidized genetic testing for obesity risk factors, coupled with access to personalized nutrition and fitness plans based on the results.
This approach moves beyond blanket recommendations, offering a more effective and sustainable path to weight management.
Improving Access to Comprehensive Care
Effective obesity management requires a holistic approach integrating lifestyle interventions, medication, and potentially bariatric surgery. Future policies must address the significant barriers to accessing comprehensive care, including affordability, geographical limitations, and a lack of trained healthcare professionals. This could involve expanding insurance coverage for obesity treatment, establishing specialized obesity clinics in underserved areas, and investing in training programs for healthcare providers specializing in obesity management.
For instance, a government-funded program could provide training stipends for physicians and nurses specializing in obesity care, increasing the availability of expert clinicians nationwide.
Technological Advancements in Obesity Prevention and Treatment
Technology offers promising avenues for obesity prevention and management. Future policies should support the development and integration of innovative technologies, such as wearable devices for monitoring physical activity and diet, telehealth platforms for remote consultations and support, and artificial intelligence (AI)-powered tools for personalized recommendations. For example, a policy could incentivize the development of AI-powered apps that provide tailored dietary advice and exercise plans based on an individual’s preferences, progress, and health data.
These technologies can enhance accessibility, engagement, and the overall effectiveness of obesity interventions.
Addressing the Social Determinants of Obesity
Obesity is deeply intertwined with socioeconomic factors, including poverty, food insecurity, and lack of access to healthy food options and safe spaces for physical activity. Future policies should prioritize addressing these social determinants through targeted interventions. For example, policies could incentivize the establishment of community gardens in low-income neighborhoods, support programs that provide access to affordable, nutritious food, and invest in the creation of safe and accessible public parks and recreational facilities.
Addressing these systemic issues is crucial for achieving lasting improvements in population-level obesity rates.
Investing in Research and Data Collection
Further research is essential to advance our understanding of obesity and develop more effective prevention and treatment strategies. Future policies should prioritize funding for research in areas such as the gut microbiome’s role in obesity, the long-term effects of various interventions, and the development of novel pharmacological agents. A national obesity research initiative, for example, could fund studies exploring the effectiveness of different dietary approaches, exercise regimens, and behavioral therapies in diverse populations, ultimately informing the development of more targeted and effective policies.
Robust data collection and analysis are also crucial for monitoring the effectiveness of existing and future policies.
Closure

Addressing the obesity epidemic requires a multi-pronged approach that tackles individual behaviors, societal influences, and the limitations of current policies. From promoting healthy lifestyles and improving access to nutritious food to leveraging technology and refining pharmaceutical interventions, progress hinges on collaborative efforts across healthcare, government, and communities. The journey towards healthier populations requires ongoing research, innovative strategies, and a sustained commitment to addressing this complex challenge.
Let’s continue the conversation and work together towards a healthier future.
Clarifying Questions
What are some common misconceptions about obesity?
Many believe obesity is solely a matter of willpower. However, genetic factors, hormonal imbalances, and environmental influences play significant roles. It’s also crucial to avoid stigmatizing language and understand that obesity is a complex medical condition.
How can I get involved in advocating for better obesity health policies?
Contact your elected officials to express your concerns and support policies that promote healthy eating, physical activity, and access to healthcare. Support organizations dedicated to obesity research and awareness. You can also participate in community initiatives promoting healthy lifestyles.
What role do schools play in addressing childhood obesity?
Schools are vital in shaping healthy habits. Implementing nutritional guidelines for school lunches, increasing physical activity programs, and providing health education are crucial steps. Parental involvement and community support are also essential.