
Ever wondered why your waistline might be a window to your overall health? We’re diving headfirst into the fascinating (and sometimes alarming!) world of obesity health concerns. From understanding the global prevalence to exploring the latest treatment strategies, we’ll unravel the complexities of this widespread issue, uncovering surprising facts and practical advice along the way. Get ready to embark on a journey of knowledge, empowering you to make informed choices about your well-being.
Obesity isn’t just about the number on the scale; it’s a multifaceted health challenge linked to a cascade of serious conditions. This exploration will cover the science behind the risks, the impact on healthcare systems, and the various strategies available for prevention and management. We’ll explore everything from lifestyle changes to medical interventions, empowering you with the knowledge to navigate this critical health concern.
Defining Obesity and its Prevalence
Obesity is a significant global health concern, impacting millions and placing a considerable strain on healthcare systems worldwide. Understanding its definition, prevalence, and contributing factors is crucial for developing effective prevention and treatment strategies.
The World Health Organization (WHO) defines obesity as an abnormal or excessive fat accumulation that presents a risk to health. This is typically assessed using the Body Mass Index (BMI), calculated as weight in kilograms divided by the square of height in meters (kg/m²).
WHO BMI Classification for Obesity
The WHO categorizes obesity based on BMI ranges. A BMI of 30 or greater is generally considered obese. Individuals with a BMI between 25 and 29.9 are classified as overweight, representing a significant risk factor for developing obesity.
BMI = weight (kg) / height (m)²
Global Obesity Prevalence
Obesity prevalence has dramatically increased globally over the past few decades. While precise figures vary depending on the data collection methods and the year, a significant portion of the world’s population is now classified as overweight or obese. This trend shows notable differences across age groups and geographical regions. Children and adolescents are experiencing a concerning rise in obesity rates, increasing their risk of developing chronic diseases later in life.
Developed nations often exhibit higher obesity rates than developing countries, although this trend is changing as urbanization and dietary shifts occur in many parts of the world. Low- and middle-income countries are seeing a rapid increase in obesity rates, often alongside the persistence of undernutrition, creating a double burden of malnutrition.
Socioeconomic Factors Contributing to Obesity
Several socioeconomic factors significantly contribute to rising obesity rates. These factors are interconnected and complex, making it challenging to isolate individual effects. However, some key contributors include:
- Reduced Physical Activity: Sedentary lifestyles, increasingly common due to urbanization and technological advancements, contribute significantly to weight gain. This includes reduced walking, cycling, and participation in physical activities.
- Unhealthy Diets: The widespread availability and affordability of processed foods, sugary drinks, and high-calorie meals contribute to increased energy intake. Marketing strategies targeting children and adolescents further exacerbate this issue.
- Socioeconomic Disparities: Access to healthy food options, safe spaces for physical activity, and healthcare services often varies across socioeconomic groups. Lower socioeconomic status is frequently associated with higher obesity rates due to limited access to resources and opportunities for healthy living.
- Environmental Factors: The built environment, including the lack of parks and safe walking areas, can influence physical activity levels. Food deserts, areas with limited access to affordable and nutritious food, also play a significant role.
Obesity Prevalence Data by Country
The following table illustrates the obesity prevalence in selected countries, highlighting variations in rates across different nations. Note that these are estimates and can vary depending on the source and year of data collection. It’s also important to understand that data collection methods differ across countries, potentially affecting comparability.
| Country | Adult Obesity Rate (%) | Child Obesity Rate (%) | Year |
|---|---|---|---|
| United States | 42 | 17 | 2023 (Estimate) |
| Mexico | 35 | 35 | 2023 (Estimate) |
| China | 16 | 11 | 2023 (Estimate) |
| United Kingdom | 28 | 20 | 2023 (Estimate) |
| India | 24 | 14 | 2023 (Estimate) |
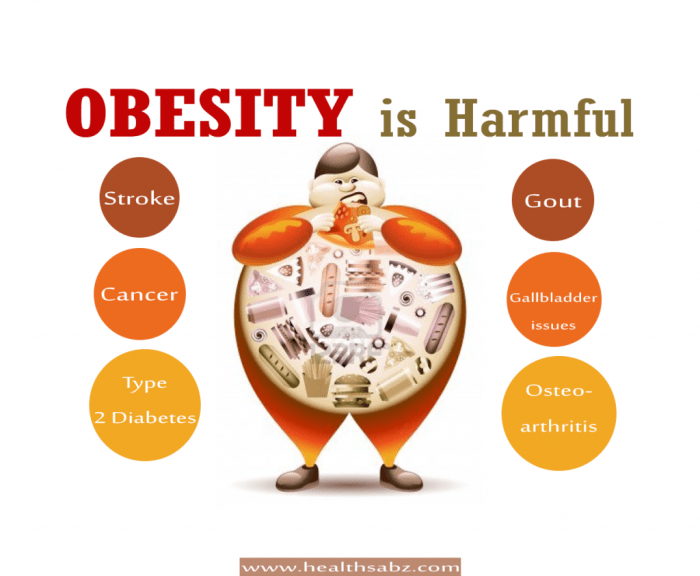
Health Risks Associated with Obesity
Obesity significantly increases the risk of developing a wide range of serious health problems. Carrying excess weight puts extra strain on various bodily systems, leading to a cascade of negative consequences that impact overall health and well-being. Understanding these risks is crucial for promoting healthier lifestyles and preventing debilitating conditions.
Obesity and Type 2 Diabetes
Obesity is a major risk factor for type 2 diabetes. Excess body fat, particularly visceral fat (fat stored around the abdominal organs), leads to insulin resistance. Insulin, a hormone produced by the pancreas, is responsible for regulating blood sugar levels. When cells become resistant to insulin, the pancreas must work harder to produce more insulin to maintain normal blood sugar levels.
Eventually, the pancreas may fail to keep up, leading to elevated blood sugar levels and the development of type 2 diabetes. This condition can lead to long-term complications such as heart disease, kidney failure, and blindness. For example, studies have shown a strong correlation between a high body mass index (BMI) and the incidence of type 2 diabetes, with individuals with obesity having a significantly higher risk compared to those with a healthy weight.
Obesity and Cardiovascular Diseases
Obesity significantly increases the risk of cardiovascular diseases (CVDs), including hypertension (high blood pressure) and coronary artery disease (CAD). Excess weight contributes to hypertension by increasing blood volume and constricting blood vessels. The added strain on the heart increases the workload, leading to an elevated risk of heart failure. Furthermore, obesity promotes the development of atherosclerosis, a condition characterized by the buildup of plaque in the arteries.
This plaque narrows the arteries, reducing blood flow to the heart and other vital organs, leading to CAD, heart attacks, and strokes. Individuals with obesity often exhibit a cluster of risk factors known as metabolic syndrome, including high blood pressure, high blood sugar, abnormal cholesterol levels, and excess abdominal fat, which further elevates their CVD risk. For instance, a study published in the “Journal of the American Medical Association” showed a strong link between obesity and increased mortality rates from CVD.
Obesity and Cancer
Obesity is linked to an increased risk of several types of cancer. The exact mechanisms are not fully understood, but several factors contribute to this association. Chronic inflammation, often associated with obesity, can damage cells and DNA, increasing the risk of cancer development. Also, hormones produced by fat tissue can influence cell growth and division, potentially promoting cancer development.
Some cancers strongly associated with obesity include colon, breast, endometrial, and kidney cancer. A large meta-analysis revealed a significant increase in the relative risk of several cancer types in obese individuals compared to those with normal weight. For example, women with obesity have a considerably higher risk of developing postmenopausal breast cancer.
Obesity and Musculoskeletal Health
Obesity places significant stress on the musculoskeletal system, particularly the joints. The extra weight increases the load on weight-bearing joints, such as the knees and hips, leading to premature wear and tear and the development of osteoarthritis. Osteoarthritis is a degenerative joint disease characterized by cartilage breakdown and joint pain. Obesity also contributes to lower back pain and increased risk of fractures.
The added strain on the spine and bones can lead to chronic pain and reduced mobility. Imagine the increased pressure on knee joints for someone significantly overweight compared to someone of a healthy weight; this extra pressure accelerates the degeneration of cartilage.
Obesity and Mental Health
Obesity is linked to an increased risk of mental health problems, including depression and anxiety. The stigma associated with obesity can lead to feelings of shame, low self-esteem, and social isolation, all of which can contribute to depression and anxiety. Furthermore, some studies suggest that hormonal imbalances and chronic inflammation associated with obesity may also play a role in the development of these mental health conditions.
The interplay between physical and mental health is complex, and addressing both is crucial for improving overall well-being in individuals with obesity. For instance, studies have shown a higher prevalence of depression and anxiety among obese individuals compared to those with normal weight.
Obesity and its Impact on Healthcare Systems
Obesity places a significant strain on healthcare systems worldwide, impacting budgets, resources, and the overall quality of care. The escalating prevalence of obesity and its associated comorbidities are driving up healthcare costs and demanding innovative solutions to address this complex challenge. Understanding the economic burden and the challenges faced by healthcare providers is crucial for developing effective strategies to mitigate the impact of obesity.
The economic burden of obesity on healthcare systems is substantial and multifaceted. It’s not simply a matter of treating obesity itself, but also the numerous health complications that often arise as a consequence. These complications, ranging from type 2 diabetes and heart disease to certain types of cancer, require extensive and costly medical interventions. Furthermore, the increased healthcare utilization associated with obesity necessitates a larger workforce, more advanced facilities, and specialized treatments, all contributing to the overall financial strain.
The Economic Burden of Obesity on Healthcare Systems
The financial impact of obesity on healthcare is staggering. It’s a global issue, with varying degrees of impact depending on the healthcare system’s structure and the prevalence of obesity within a given population. The costs are not limited to direct medical expenses; they also include indirect costs like lost productivity due to illness and disability. For example, a study by the OECD (Organisation for Economic Co-operation and Development) found a strong correlation between obesity prevalence and healthcare expenditure across member countries.
This means countries with higher obesity rates tend to spend more on healthcare, often exceeding the costs associated with other major health concerns.
- Direct Medical Costs: These include expenses related to diagnosis, treatment, and management of obesity and its associated conditions such as diabetes, hypertension, and cardiovascular disease. This encompasses doctor visits, hospital stays, medications, and surgical procedures.
- Indirect Costs: These encompass lost productivity due to illness and disability, absenteeism from work, and reduced overall economic output. The impact on the workforce is significant, with obese individuals often facing higher rates of sick leave and reduced work capacity.
- Long-term Care Costs: Obesity significantly increases the risk of long-term disability and the need for ongoing care, including nursing home placement. These long-term care costs contribute substantially to the overall economic burden.
Increased Healthcare Utilization Associated with Obesity-Related Complications
Individuals with obesity frequently require more healthcare services than their healthier counterparts. This increased utilization stems from the higher risk of developing numerous chronic diseases. For instance, someone with obesity-related type 2 diabetes might need regular blood glucose monitoring, medication management, and potential hospitalizations for complications like diabetic ketoacidosis. Similarly, those with obesity-related cardiovascular disease might require more frequent check-ups, cardiac rehabilitation, and potentially even coronary bypass surgery.
This higher frequency of appointments, tests, and treatments directly contributes to the escalating healthcare costs associated with obesity.
Challenges Faced by Healthcare Providers in Managing Obesity Effectively
Healthcare providers face numerous challenges in effectively managing obesity. These challenges are complex and interconnected, requiring a multi-pronged approach to tackle them successfully. The lack of a single, universally effective treatment contributes significantly to the difficulty.
One major hurdle is the complexity of obesity itself. It’s not simply a matter of willpower; it’s influenced by genetic predisposition, environmental factors, socioeconomic status, and psychological factors. Effectively addressing these multifaceted influences requires a collaborative, patient-centered approach involving healthcare professionals from various disciplines. Furthermore, long-term lifestyle changes, such as adopting a healthy diet and engaging in regular physical activity, are challenging to maintain, requiring ongoing support and motivation.
The lack of adequate resources and reimbursement policies for comprehensive obesity management programs further exacerbates the challenges faced by healthcare providers.
Treatment and Management Strategies for Obesity
Tackling obesity requires a multifaceted approach, combining lifestyle modifications with potential medical interventions. Success hinges on a personalized strategy tailored to individual needs and preferences, acknowledging that there’s no one-size-fits-all solution. The journey towards healthier weight involves commitment, patience, and a supportive environment.
Dietary Changes
Effective weight management begins with a balanced and nutritious diet. This involves consuming a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting processed foods, sugary drinks, and excessive unhealthy fats. Portion control is crucial; understanding serving sizes helps prevent overeating. Registered dietitians can provide personalized guidance on creating a sustainable meal plan that aligns with individual dietary needs and preferences.
For example, swapping sugary sodas for water or unsweetened tea can significantly reduce daily calorie intake. Similarly, choosing grilled chicken over fried chicken reduces fat and calorie consumption.
Exercise and Physical Activity
Regular physical activity is essential for weight loss and overall health. The recommended amount of exercise is at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities twice a week. Activities can range from brisk walking and cycling to swimming and team sports. Finding activities one enjoys increases adherence to the exercise regimen.
For instance, someone who enjoys dancing might incorporate dance classes into their routine, while someone who prefers hiking might choose weekly hikes in a nearby park. The key is consistency and finding enjoyable forms of movement.
Behavioral Therapy
Behavioral therapy plays a vital role in long-term weight management. It addresses underlying psychological factors contributing to overeating, such as emotional eating or stress-related eating habits. Techniques like cognitive behavioral therapy (CBT) help individuals identify and modify unhealthy eating patterns and develop coping mechanisms for emotional challenges. For example, CBT can help someone recognize triggers that lead to emotional eating and develop strategies to manage those triggers, such as engaging in relaxation techniques instead of turning to food.
Medication in Obesity Management
Certain medications can assist with weight loss, particularly when combined with lifestyle modifications. These medications may work by suppressing appetite, increasing satiety, or affecting how the body absorbs fat. However, medications are generally used as an adjunct to lifestyle changes, not as a standalone solution. The choice of medication depends on individual health conditions and potential side effects.
A healthcare professional should carefully assess individual needs and potential risks before prescribing any medication for weight loss. For instance, some medications may increase heart rate or blood pressure, requiring careful monitoring.
Bariatric Surgery
Bariatric surgery is a surgical intervention for individuals with severe obesity (BMI ≥ 40 or BMI ≥ 35 with obesity-related health problems). These procedures restrict food intake or alter the digestive process, leading to significant weight loss. However, bariatric surgery carries risks, including infection, bleeding, and potential complications. It requires a comprehensive pre-operative assessment and post-operative care.
The long-term success of bariatric surgery depends on adherence to lifestyle changes, including dietary modifications and regular exercise. For example, gastric bypass surgery reduces the size of the stomach and alters the digestive pathway, leading to significant weight loss. However, individuals undergoing this surgery need to carefully follow a post-operative diet to avoid complications.
Weight Loss Programs: A Comparison
Various weight loss programs exist, each with its own approach and effectiveness. Commercial programs often provide structured meal plans, exercise routines, and support groups. However, their effectiveness varies, and some may not be sustainable in the long run. Individualized programs designed by healthcare professionals, such as registered dietitians and physicians, offer tailored strategies based on individual needs and preferences.
The effectiveness of any weight loss program depends on individual commitment and adherence to the plan. For example, some programs may focus heavily on calorie restriction, while others may emphasize behavioral modification. The best program is one that suits the individual’s lifestyle and preferences.
Sample Weekly Meal Plan for Weight Loss
This sample meal plan provides a balanced approach with approximately 1200-1500 calories per day. Consult a registered dietitian for a personalized plan.
| Day | Breakfast | Lunch | Dinner |
|---|---|---|---|
| Monday | Oatmeal with berries and nuts | Salad with grilled chicken or fish | Baked salmon with roasted vegetables |
| Tuesday | Greek yogurt with fruit | Lentil soup with whole-wheat bread | Chicken stir-fry with brown rice |
| Wednesday | Scrambled eggs with spinach and whole-wheat toast | Turkey breast sandwich on whole-wheat bread with lettuce and tomato | Lean ground beef with sweet potato and green beans |
| Thursday | Smoothie with fruits, vegetables, and protein powder | Leftovers from dinner | Vegetarian chili with cornbread |
| Friday | Whole-wheat pancakes with fruit | Tuna salad with whole-wheat crackers | Chicken breast with quinoa and steamed broccoli |
| Saturday | Breakfast burrito with eggs, beans, and vegetables | Large salad with chickpeas and feta cheese | Pizza with whole-wheat crust, vegetables, and lean protein |
| Sunday | French toast made with whole-wheat bread | Leftovers from dinner | Roast chicken with roasted potatoes and carrots |
The Role of Pharmacy in Obesity Management
Pharmacists are uniquely positioned to play a crucial role in the fight against obesity, offering a readily accessible point of contact for patients seeking support and guidance. Their expertise in medication, patient counseling, and health promotion makes them invaluable members of the multidisciplinary obesity management team. They can significantly impact patient outcomes by improving medication adherence, promoting healthy lifestyle changes, and coordinating care with other healthcare providers.Pharmacists’ Contributions to Obesity Management
Medication Dispensing and Counseling
Pharmacists dispense a range of medications used in obesity management, including appetite suppressants (such as phentermine or liraglutide), and medications that affect fat absorption (such as orlistat). Beyond dispensing, they provide crucial counseling on the proper use of these medications, including potential side effects, drug interactions, and monitoring strategies. This includes explaining the importance of adhering to prescribed dosages and reporting any adverse effects promptly.
For example, a pharmacist might explain that orlistat can cause gastrointestinal issues and recommend strategies for mitigating these side effects, such as adjusting dietary fat intake.
Patient Counseling Strategies for Adherence
Effective communication is paramount in ensuring patient adherence to weight management plans. Pharmacists employ various strategies to enhance adherence. These include motivational interviewing techniques, providing clear and concise instructions, tailoring information to individual patient needs and health literacy levels, and utilizing medication organizers or reminder systems. For example, a pharmacist might actively listen to a patient’s concerns about medication side effects and collaboratively develop a plan to address those concerns.
They may also demonstrate the use of a medication dispenser and schedule regular follow-up appointments to reinforce positive behavior and monitor progress.
Education on Healthy Lifestyle Choices and Resources
Pharmacists are key educators, providing patients with information on healthy eating habits, physical activity recommendations, and stress management techniques. They can also connect patients with community resources such as weight loss programs, support groups, and nutrition counseling services. For instance, a pharmacist could provide pamphlets on healthy meal planning, explain the benefits of regular exercise, and offer details on local fitness centers or community walks.
They might also guide patients towards reputable online resources for verified nutrition information.
Collaboration in a Multidisciplinary Approach
Pharmacists contribute significantly to the multidisciplinary approach to obesity management by collaborating effectively with physicians, dieticians, and other healthcare professionals. This collaborative care model ensures comprehensive patient care and improves outcomes. For example, a pharmacist might communicate with a patient’s physician regarding medication efficacy and any observed side effects, allowing for timely adjustments to the treatment plan. They could also work with a dietician to ensure medication choices align with the patient’s dietary plan, minimizing potential drug-diet interactions and maximizing treatment success.
This coordinated effort helps create a holistic and effective approach to weight management.
Prevention and Public Health Initiatives
Preventing obesity requires a multifaceted approach encompassing individual choices and broader societal changes. Addressing this complex issue demands a comprehensive strategy targeting various aspects of life, from individual dietary habits and physical activity levels to the environmental factors influencing these behaviors. Effective prevention hinges on a collaborative effort between individuals, communities, and governments.Effective public health strategies are crucial for curbing the rising rates of childhood obesity.
These strategies must be implemented early, targeting children and their families, and focus on fostering healthy habits that last a lifetime.
Effective Public Health Strategies for Preventing Childhood Obesity
A successful strategy involves a combination of approaches. For example, implementing school-based nutrition programs that provide healthy meals and snacks can significantly impact children’s dietary intake. These programs can also incorporate nutrition education, teaching children about healthy eating choices and portion control. Simultaneously, increasing physical activity opportunities in schools, such as mandatory recess and physical education classes, is vital.
Community-based initiatives, like safe parks and recreational facilities, can extend these opportunities beyond school hours. Furthermore, encouraging families to adopt healthier lifestyles through community-based workshops and support groups can create a supportive environment for change. These combined efforts can create a significant impact on childhood obesity rates.
The Importance of Nutrition Education in Preventing Obesity
Nutrition education plays a pivotal role in preventing obesity. By equipping individuals with the knowledge and skills to make informed food choices, we empower them to control their weight and overall health. Effective nutrition education programs should focus on teaching about balanced diets, portion sizes, and the nutritional value of different foods. These programs should also address the influence of marketing and advertising on food choices, empowering individuals to make healthier selections despite the pressures of modern consumerism.
Practical skills, such as meal planning and cooking healthy meals, should also be incorporated. A successful nutrition education program considers the cultural background and socioeconomic status of the target audience, tailoring the information to ensure it is accessible and relevant. For example, a program targeted at low-income families might include information on affordable, nutritious food options and cooking techniques.
Community-Based Programs Promoting Physical Activity
Community-based programs are essential for promoting physical activity and combating sedentary lifestyles. These programs can take many forms, from creating safe and accessible walking and biking paths to organizing community sports leagues and fitness classes. Examples include the creation of neighborhood parks with playgrounds and exercise equipment, the establishment of walking clubs, and the implementation of community-wide fitness challenges.
The success of these programs depends on their accessibility and appeal to diverse populations. Programs should consider factors like geographical location, cultural preferences, and socioeconomic status to ensure they are inclusive and reach the widest possible audience. Successful programs often incorporate elements of fun and social interaction to encourage participation and long-term engagement.
Government Policies and Regulations Supporting Obesity Prevention Efforts
Government intervention plays a crucial role in creating an environment that supports healthy choices. Policies such as taxes on sugary drinks and unhealthy foods can discourage consumption of these items. Conversely, subsidies for fruits and vegetables can make healthier options more affordable and accessible. Regulations concerning food labeling and marketing can provide consumers with clearer information about the nutritional content of products and limit the exposure of children to unhealthy food advertising.
Furthermore, policies promoting physical activity, such as investments in public transportation and the creation of pedestrian-friendly infrastructure, can encourage active lifestyles. Stronger regulations on food marketing directed at children are also crucial, protecting them from manipulative advertising tactics.
Key Recommendations for Preventing Obesity
Preventing obesity requires a comprehensive strategy involving individual responsibility and broader societal changes. Here are key recommendations:
- Promote breastfeeding for infants.
- Encourage healthy eating habits from an early age.
- Limit screen time and encourage regular physical activity.
- Make healthy food options readily available and affordable.
- Implement effective nutrition education programs in schools and communities.
- Create supportive environments that encourage physical activity.
- Support government policies that promote healthy eating and active living.
- Address socioeconomic factors that contribute to obesity.
- Provide access to affordable and quality healthcare services for obesity management.
- Promote research and innovation in obesity prevention and treatment.
Illustrative Examples of Obesity-Related Complications
Obesity significantly increases the risk of developing a range of serious health complications. Understanding the physiological mechanisms underlying these complications is crucial for effective prevention and treatment strategies. The following examples illustrate the intricate connections between excess body fat and the development of type 2 diabetes, atherosclerosis, and osteoarthritis.
Type 2 Diabetes Mellitus and Obesity
Obesity is a major risk factor for type 2 diabetes, a chronic metabolic disorder characterized by high blood sugar levels. The link between the two is complex and involves multiple pathways. Excess adipose tissue, particularly visceral fat (fat surrounding internal organs), leads to insulin resistance. This means the body’s cells become less responsive to insulin, a hormone that regulates blood glucose.
Consequently, glucose accumulates in the bloodstream, leading to hyperglycemia.
Physiological Mechanisms:
1. Increased Free Fatty Acids: Excess adipose tissue releases high levels of free fatty acids into the bloodstream. These fatty acids interfere with insulin signaling pathways in muscle, liver, and fat cells, reducing their ability to uptake glucose.
2. Inflammation: Adipose tissue in obese individuals is often inflamed, releasing inflammatory cytokines. These cytokines further impair insulin signaling and contribute to insulin resistance.
3. Adipokines Imbalance: Adipose tissue secretes various hormones called adipokines. In obesity, the balance of these adipokines is disrupted. For example, decreased levels of adiponectin (an insulin-sensitizing adipokine) and increased levels of leptin (a hormone that regulates appetite) contribute to insulin resistance and hyperglycemia.
4. Beta-Cell Dysfunction: Over time, the pancreas, which produces insulin, may become overworked and less efficient. This leads to beta-cell dysfunction, further exacerbating hyperglycemia.
Illustrative Description: Imagine a key (insulin) trying to open a lock (cell receptor). In a healthy individual, the key fits perfectly, allowing glucose to enter the cell. In obesity, the lock mechanism is jammed by excess free fatty acids and inflammatory molecules, hindering the key’s ability to unlock the cell. Glucose remains outside the cell, leading to high blood sugar levels.
Atherosclerosis and Obesity
Obesity accelerates the development of atherosclerosis, a condition characterized by the buildup of plaque within the artery walls. This plaque, composed of cholesterol, fats, calcium, and other substances, narrows the arteries, reducing blood flow and increasing the risk of heart attack and stroke.
Development in Obese Individuals:
1. Increased LDL Cholesterol: Obesity often leads to elevated levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol. High LDL cholesterol contributes significantly to plaque formation.
2. Inflammation: As with type 2 diabetes, chronic inflammation associated with obesity plays a crucial role in atherosclerosis. Inflammatory cells infiltrate the artery walls, promoting plaque formation.
3. Endothelial Dysfunction: Obesity can damage the endothelium, the inner lining of the arteries. This damage makes the arteries more susceptible to plaque buildup.
4. Oxidative Stress: Obesity increases oxidative stress, an imbalance between the production of free radicals and the body’s ability to neutralize them. Oxidative stress damages the artery walls and contributes to plaque formation.
Illustrative Description: Imagine a pipe (artery) gradually becoming clogged with sticky substances (plaque). In an obese individual, the pipe is more prone to clogging due to high levels of cholesterol and inflammation. The narrowing of the pipe restricts the flow of water (blood), potentially leading to a blockage (heart attack or stroke).
Osteoarthritis and Obesity
Obesity is a major risk factor for osteoarthritis, a degenerative joint disease characterized by cartilage breakdown and joint pain. Excess weight places increased stress on weight-bearing joints, accelerating cartilage degradation.
Development in Obese Individuals:
1. Increased Joint Load: Extra weight significantly increases the load on weight-bearing joints like knees and hips, leading to excessive wear and tear on the cartilage.
2. Biomechanical Stress: Obesity alters joint biomechanics, leading to abnormal joint loading and increased stress on the cartilage.
3. Inflammation: Adipose tissue releases inflammatory molecules that contribute to cartilage degradation and joint inflammation.
4. Cartilage Damage: The combination of increased mechanical stress and inflammation leads to progressive cartilage damage, eventually resulting in pain, stiffness, and limited joint mobility.
Illustrative Description: Imagine a cushion (cartilage) protecting two bones in a joint. In an obese individual, the extra weight compresses the cushion excessively, causing it to wear down faster. The resulting friction between the bones leads to pain and inflammation.
Epilogue

So, as we wrap up our deep dive into obesity health concerns, remember this: it’s a journey, not a race. While the statistics can be daunting, the power to make positive changes lies within each of us. By understanding the risks, embracing healthy lifestyle choices, and seeking support when needed, we can collectively tackle this global challenge and pave the way for healthier, happier lives.
Let’s make informed decisions and prioritize our well-being – one step at a time!
FAQ Corner
What is the difference between overweight and obese?
Overweight refers to having excess body weight for a particular height, often measured using BMI. Obesity is a more severe condition characterized by an excessive accumulation of body fat that poses significant health risks.
Can obesity be reversed?
While complete reversal might be challenging, significant weight loss through lifestyle changes and medical interventions is possible, leading to improved health outcomes and reduced risks.
Are all weight loss programs created equal?
Absolutely not! Effectiveness varies widely. Programs that combine diet, exercise, and behavioral support tend to yield better and more sustainable results than quick-fix diets.
What role does genetics play in obesity?
Genetics can influence an individual’s predisposition to weight gain, but lifestyle factors like diet and exercise play a much larger role in determining body weight and overall health.

