Ever wondered how those extra pounds impact your body and mind? We’re diving headfirst into the fascinating – and sometimes alarming – world of obesity health issues. From the science behind the bulge to the emotional rollercoaster it can create, we’ll unpack the complexities of this widespread concern. Get ready for an engaging journey of discovery!
Obesity, defined by a Body Mass Index (BMI) over 30, affects millions globally, impacting not just physical health but also mental well-being. We’ll explore the intricate links between obesity and conditions like heart disease, type 2 diabetes, and depression, examining the underlying mechanisms and highlighting the latest research. We’ll also discuss effective treatment strategies, including lifestyle changes, medication, and surgery, empowering you with the knowledge to make informed decisions about your health.
Defining Obesity and its Prevalence
Obesity is a significant global health concern, impacting millions and placing a substantial strain on healthcare systems worldwide. Understanding its definition and prevalence is crucial for effective prevention and treatment strategies.Obesity is generally defined as an abnormal or excessive fat accumulation that presents a risk to health. It’s most commonly assessed using the Body Mass Index (BMI), calculated as weight in kilograms divided by the square of height in meters (kg/m²).
While BMI isn’t a perfect measure, it provides a useful screening tool. Classifications typically include: Underweight ( <18.5 kg/m²), Normal weight (18.5-24.9 kg/m²), Overweight (25.0-29.9 kg/m²), and Obese (≥30 kg/m²). Further classifications within obesity exist (e.g., Class I, Class II, Class III obesity), reflecting increasing levels of severity. It's important to remember that BMI doesn't account for factors like muscle mass, bone density, or body fat distribution, and therefore should be interpreted cautiously.
Global and Regional Obesity Prevalence
The global prevalence of obesity has dramatically increased in recent decades. Data from the World Health Organization (WHO) and other reputable sources show a significant rise across numerous countries and regions. For example, the WHO estimates that globally, over 1.9 billion adults were overweight in 2016, with over 650 million classified as obese.
This represents a substantial increase compared to previous decades. Prevalence varies considerably across different regions, with some experiencing more rapid increases than others. Developed nations often show higher rates of obesity, though rapid economic growth in some developing nations is also leading to a surge in obesity prevalence. Variations also exist within countries, often linked to socioeconomic factors and access to healthcare.
For instance, obesity rates might be higher in lower socioeconomic groups due to limited access to healthy food options and increased exposure to processed foods high in sugar and fat. Additionally, certain ethnic groups may have a higher predisposition to obesity based on genetic and lifestyle factors.
Obesity Rates Across Demographics
The following table illustrates the variability of obesity rates across different age groups and socioeconomic strata. Note that these are illustrative examples, and precise figures vary based on the specific study and population sampled. The data presented is representative of general trends and should not be considered exhaustive.
| Demographic Group | Obesity Prevalence (Illustrative Example) | Contributing Factors | Regional Variations (Illustrative Example) |
|---|---|---|---|
| Adults (30-49 years) | 35% | Sedentary lifestyles, unhealthy diets | Higher in North America, lower in some parts of Africa |
| Children (5-17 years) | 15% | Increased consumption of processed foods, lack of physical activity | Significant increases observed in many developing nations |
| Low Socioeconomic Status | 40% | Limited access to healthy foods, higher stress levels | Marked disparities within urban and rural areas |
| High Socioeconomic Status | 25% | Unhealthy dietary patterns despite access to resources | Regional variations less pronounced than in lower socioeconomic groups |
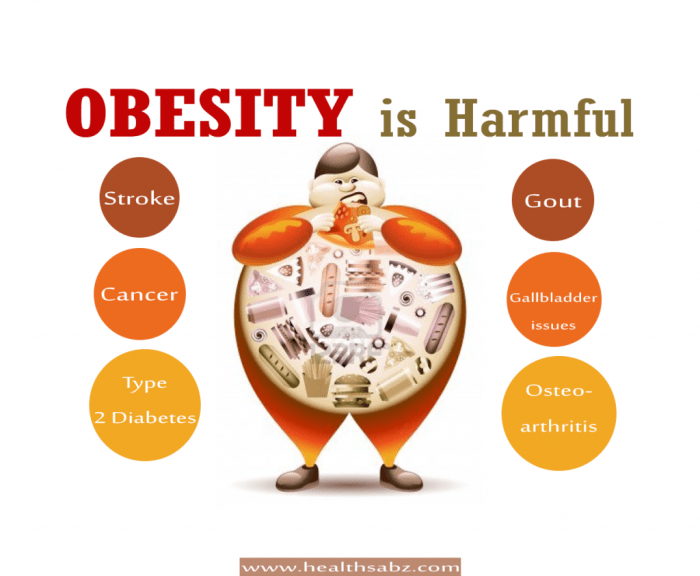
Physical Health Complications of Obesity

Carrying excess weight significantly increases the risk of developing a range of serious health problems. These complications arise from the body’s physiological response to chronic energy imbalance and the subsequent inflammatory processes. Understanding these links is crucial for promoting healthy lifestyles and effective preventative measures.
Cardiovascular Diseases
Obesity is a major risk factor for cardiovascular diseases (CVDs), a group of disorders affecting the heart and blood vessels. The extra weight strains the heart, leading to increased blood pressure and cholesterol levels. This increased workload can cause the heart muscle to weaken and become less efficient, potentially resulting in heart failure. Furthermore, obesity promotes the formation of blood clots, which can travel to the brain and cause a stroke, a life-threatening event disrupting blood flow to the brain.
The link is so strong that individuals with obesity often experience premature aging of their cardiovascular system. For example, a 45-year-old individual with severe obesity may have the cardiovascular health profile of a 60-year-old of normal weight.
Type 2 Diabetes
Obesity is strongly associated with type 2 diabetes, a metabolic disorder characterized by high blood sugar levels. Excess fat, particularly visceral fat (fat surrounding the organs), interferes with the body’s ability to use insulin effectively. Insulin is a hormone that helps glucose (sugar) enter cells for energy. When insulin resistance develops, glucose builds up in the bloodstream, leading to high blood sugar levels and eventually type 2 diabetes.
This process is often gradual, starting with prediabetes, a condition where blood sugar levels are higher than normal but not yet diabetic. The mechanism involves a complex interplay of hormones and inflammatory responses within the fat tissue and the liver, ultimately leading to impaired glucose metabolism.
Musculoskeletal Problems
The extra weight carried by obese individuals puts significant stress on their joints and bones. This increased load can accelerate the degeneration of cartilage, leading to osteoarthritis, a painful condition affecting the joints. The knees, hips, and spine are particularly vulnerable. Obesity also contributes to back pain, as the added weight strains the muscles and ligaments supporting the spine.
The combination of joint pain and reduced mobility often leads to decreased physical activity, further exacerbating the problem and creating a vicious cycle. For instance, individuals with severe osteoarthritis may experience significant limitations in their daily activities, impacting their quality of life considerably.
Other Physical Health Issues
Obesity is linked to a wide range of other health problems.
- Sleep Apnea: Excess weight can obstruct the airways during sleep, leading to pauses in breathing and disrupted sleep patterns.
- Certain Cancers: Obesity is associated with an increased risk of several types of cancer, including colon, breast, endometrial, and kidney cancer. The exact mechanisms are still under investigation, but chronic inflammation and hormonal imbalances are likely contributors.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Excess fat accumulation in the liver can cause inflammation and damage, potentially leading to cirrhosis and liver failure. NAFLD is becoming increasingly common alongside the rise in obesity rates.
- Gallstones: Obesity increases the risk of developing gallstones, small, hard deposits that form in the gallbladder.
- Gout: This painful form of arthritis is more common in obese individuals due to altered metabolism and increased uric acid levels.
Mental Health Aspects of Obesity
Obesity significantly impacts mental well-being, creating a complex interplay between physical and psychological health. The stigma associated with weight, coupled with the physiological effects of excess weight, contributes to a range of mental health challenges. Understanding this connection is crucial for developing effective interventions and promoting holistic well-being.
Obesity and Depression
Research consistently demonstrates a strong correlation between obesity and depression. Individuals with obesity are more likely to experience depressive symptoms and disorders than those with a healthy weight. This isn’t simply a matter of correlation; studies suggest a bidirectional relationship. For instance, inflammation, a common consequence of obesity, can affect brain function and increase the risk of depression.
Conversely, depression can lead to decreased physical activity, unhealthy eating habits, and weight gain, further exacerbating the cycle. Studies using large datasets, like those from national health surveys, consistently show a statistically significant association between higher BMI and increased prevalence of depressive disorders, diagnosed through standardized clinical assessments. This link highlights the importance of integrated care approaches that address both physical and mental health needs simultaneously.
Impact on Self-Esteem and Body Image
Obesity often negatively affects self-esteem and body image. Societal beauty standards frequently prioritize thinness, leading individuals with obesity to experience feelings of inadequacy, shame, and low self-worth. Internalized negative messages from media, peers, and even family members can further erode self-esteem. This can manifest in various ways, including social withdrawal, avoidance of activities that involve physical exposure, and difficulty forming and maintaining healthy relationships.
The constant barrage of unrealistic body ideals presented in popular culture contributes to this pervasive issue, making it vital to promote realistic and diverse representations of beauty.
Social Stigma and Discrimination
The social stigma surrounding obesity is a significant contributor to poor mental health. Obese individuals frequently face prejudice, discrimination, and bias in various aspects of life, including employment, healthcare, and social interactions. This can lead to feelings of isolation, marginalization, and increased stress levels, further impacting mental well-being. Studies have shown that obese individuals report higher rates of experiencing weight-based discrimination in various settings, ranging from job interviews to interactions with healthcare providers.
This discrimination can create a vicious cycle, where individuals internalize negative stereotypes and engage in self-stigmatizing behaviors.
Strategies for Promoting Positive Body Image and Mental Well-being
Promoting positive body image and mental well-being in obese populations requires a multi-faceted approach. This includes:
- Promoting body acceptance: Encouraging individuals to appreciate their bodies for their functionality rather than solely focusing on appearance. This involves challenging societal beauty standards and fostering self-compassion.
- Mindfulness and self-care practices: Implementing techniques such as meditation, yoga, or other relaxation methods to manage stress and improve emotional regulation.
- Cognitive behavioral therapy (CBT): CBT can help individuals identify and challenge negative thought patterns and beliefs about their bodies and weight.
- Social support and community building: Creating supportive environments where individuals feel accepted and understood, reducing feelings of isolation and shame.
- Addressing weight bias in healthcare settings: Training healthcare professionals to provide compassionate and non-judgmental care to obese individuals, avoiding stigmatizing language and practices.
Obesity Treatment and Management Strategies

Tackling obesity requires a multifaceted approach, combining lifestyle modifications with potential medical interventions. The most effective strategies are personalized, considering individual factors like age, health conditions, and personal preferences. Success hinges on a long-term commitment to healthy habits and consistent effort.
Lifestyle Interventions for Weight Management
Lifestyle changes form the cornerstone of obesity treatment, particularly for those with mild to moderate obesity. These interventions focus on sustainable dietary adjustments and regular physical activity. Significant and lasting weight loss often requires a combined approach.
Dietary recommendations typically involve reducing calorie intake, focusing on nutrient-dense foods, and limiting processed foods, sugary drinks, and unhealthy fats. Portion control is crucial. A balanced diet rich in fruits, vegetables, whole grains, and lean protein is essential. Registered dietitians can provide personalized guidance on creating a suitable meal plan.
Regular physical activity is equally vital. The recommended amount is at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week, along with muscle-strengthening activities twice a week. This can include brisk walking, jogging, swimming, cycling, or other activities enjoyable to the individual. Finding activities that are enjoyable and sustainable is key to long-term adherence.
Bariatric Surgery
For individuals with severe obesity (BMI ≥40 or BMI ≥35 with obesity-related health complications), bariatric surgery may be considered. These procedures aim to restrict food intake or alter the digestive process, leading to significant weight loss.
Several types of bariatric surgery exist, including gastric bypass, sleeve gastrectomy, and adjustable gastric banding. Gastric bypass alters the digestive tract, reducing food absorption. Sleeve gastrectomy removes a portion of the stomach, reducing its capacity. Adjustable gastric banding restricts stomach size with an inflatable band. The choice of procedure depends on individual factors and surgeon recommendations.
Post-operative care is crucial, involving dietary changes, regular monitoring, and often lifelong follow-up.
Pharmacological Interventions for Weight Loss
Pharmacological interventions can complement lifestyle changes, particularly for individuals who haven’t achieved significant weight loss through lifestyle modifications alone. Several drug classes are available, each with its mechanism of action and potential side effects.
Some medications suppress appetite, while others affect nutrient absorption or increase metabolism. Examples include liraglutide (a GLP-1 receptor agonist), orlistat (a lipase inhibitor), and phentermine (an appetite suppressant). These medications are usually prescribed by a doctor and should be used under medical supervision. The effectiveness and side effects vary depending on the individual and the specific medication.
Comparison of Obesity Treatment Options
| Treatment Option | Effectiveness | Side Effects | Suitability |
|---|---|---|---|
| Lifestyle Interventions (Diet & Exercise) | Moderate to high, depending on adherence | Generally mild (e.g., muscle soreness, fatigue) | Suitable for most individuals with mild to moderate obesity |
| Bariatric Surgery | High, often leading to significant and sustained weight loss | Can include surgical complications, nutrient deficiencies, and potential long-term side effects | Suitable for individuals with severe obesity (BMI ≥40 or BMI ≥35 with obesity-related complications) |
| Pharmacological Interventions | Moderate, often enhances weight loss when combined with lifestyle changes | Vary widely depending on the medication; can include nausea, diarrhea, constipation, headache, etc. | Suitable for individuals who haven’t achieved significant weight loss with lifestyle changes alone, under medical supervision. |
The Role of Pharmacy in Obesity Management
Pharmacists are uniquely positioned to play a crucial role in the management of obesity, extending beyond simply dispensing medications. Their accessibility, expertise in medication management, and patient counseling skills make them vital members of the interdisciplinary obesity care team. They can significantly impact patient outcomes by improving medication adherence, educating patients on lifestyle changes, and proactively identifying and managing potential side effects.
Pharmacist’s Role in Patient Education
Pharmacists provide essential education on weight management medications, explaining their mechanisms of action, potential benefits, and risks. This includes discussing common side effects, how to manage them, and when to seek medical attention. Beyond medication, pharmacists also educate patients on lifestyle modifications crucial for successful weight loss, such as balanced nutrition, regular physical activity, stress management techniques, and behavioral strategies.
This education empowers patients to make informed choices and actively participate in their treatment plan. For example, a pharmacist might explain the difference between different types of weight-loss medications, like GLP-1 receptor agonists and lipase inhibitors, highlighting the benefits and drawbacks of each to help patients make an informed decision in consultation with their physician.
Pharmacist’s Contribution to Medication Adherence and Side Effect Monitoring
Medication adherence is a major challenge in chronic disease management, including obesity. Pharmacists actively contribute by providing clear instructions, addressing concerns about side effects, and monitoring medication effectiveness. They can use various techniques to improve adherence, such as providing pill organizers, offering counseling sessions, and utilizing technology-based reminders. Furthermore, pharmacists play a crucial role in identifying and managing potential side effects, ensuring early intervention to prevent serious complications.
For instance, if a patient is experiencing nausea from a weight-loss medication, the pharmacist can suggest strategies to mitigate this side effect, like taking the medication with food or adjusting the dosage under the guidance of the prescribing physician.
Importance of Pharmacist-Patient Communication
Open and effective communication between pharmacists and patients is paramount for successful weight management. Pharmacists create a safe and supportive environment where patients feel comfortable discussing their concerns, challenges, and progress. Active listening, empathetic responses, and motivational interviewing techniques are essential to build trust and encourage patient engagement. Regular check-ins and follow-up appointments help track progress, address emerging issues, and reinforce positive behaviors.
For example, a pharmacist might use motivational interviewing to help a patient overcome feelings of discouragement after a setback, focusing on past successes and setting realistic future goals.
Examples of Pharmacy-Based Programs
Many pharmacies are implementing programs specifically designed to support weight loss and overall health. These initiatives often include group weight-loss support sessions, workshops on healthy eating and exercise, medication management programs, and collaborations with other healthcare professionals, such as dietitians and exercise physiologists. Some pharmacies offer personalized weight management plans tailored to individual patient needs, incorporating medication, lifestyle changes, and regular monitoring.
For example, a pharmacy might partner with a local gym to offer discounted memberships to patients participating in their weight-loss program.
Specific Actions Pharmacists Can Take
Pharmacists can take several proactive steps to support patients with obesity.
- Provide comprehensive medication counseling, including information on benefits, risks, and side effects.
- Offer strategies for improving medication adherence, such as pill organizers or reminder systems.
- Educate patients on lifestyle modifications, such as healthy eating, regular exercise, and stress management.
- Monitor for potential side effects and intervene promptly to prevent complications.
- Conduct regular follow-up appointments to track progress and address concerns.
- Refer patients to other healthcare professionals, such as dietitians, exercise physiologists, or mental health specialists, as needed.
- Promote and participate in pharmacy-based weight management programs.
- Utilize technology, such as mobile apps or telehealth platforms, to enhance patient engagement and support.
Long-Term Health Outcomes and Prevention
Untreated obesity casts a long shadow, significantly impacting lifespan and quality of life. The cumulative effects of excess weight on various organ systems lead to a cascade of health problems, ultimately increasing the risk of premature death. Understanding these long-term consequences is crucial for implementing effective prevention strategies.
Long-Term Health Consequences of Untreated Obesity
Obesity significantly increases the risk of developing numerous chronic diseases. These include type 2 diabetes, cardiovascular disease (including heart attacks and strokes), certain types of cancer (endometrial, breast, colon, kidney, and liver), osteoarthritis, sleep apnea, and non-alcoholic fatty liver disease (NAFLD). The increased strain on the body’s systems, coupled with chronic inflammation, accelerates the aging process and elevates the risk of premature mortality.
For example, studies consistently show that individuals with a body mass index (BMI) over 30 have a substantially higher risk of dying prematurely compared to those with a healthy BMI. The increased risk isn’t just limited to one or two conditions; it’s a multifaceted increase in the likelihood of experiencing multiple debilitating health issues.
Preventing Obesity in Children and Adolescents
Early intervention is key to preventing obesity. Education plays a vital role, focusing on healthy eating habits and regular physical activity. This includes teaching children about portion control, the importance of consuming fruits and vegetables, and limiting sugary drinks and processed foods. Schools can contribute significantly by offering nutritious meals, incorporating physical education into the curriculum, and promoting healthy lifestyle choices through educational programs.
Parental involvement is crucial; parents need to model healthy behaviors and create a supportive environment that encourages physical activity and healthy food choices. For instance, family meals together, where healthy options are presented, can be a powerful tool in shaping long-term eating habits.
Community-Level Public Health Initiatives
Combating obesity requires a multi-pronged approach at the community level. This includes implementing policies that promote access to healthy, affordable food options, particularly in underserved communities. Creating safe and accessible spaces for physical activity, such as parks and recreational facilities, is equally important. Public awareness campaigns can educate the public about the risks of obesity and promote healthy lifestyle choices.
Furthermore, initiatives that support community gardens and farmers’ markets can increase access to fresh produce. Successful examples include initiatives that have transformed urban spaces into walkable and bikeable areas, increasing physical activity and reducing reliance on cars. These combined efforts create a supportive environment that fosters healthy behaviors.
Visual Representation of Long-Term Obesity Impact
Imagine a diagram showing a human body divided into sections representing major organ systems: the heart, lungs, liver, kidneys, and joints. Each section initially shows a healthy, functioning organ. As you move along the timeline of the diagram, representing years of untreated obesity, the healthy organs gradually become stressed and diseased. The heart section might show thickening of the heart muscle and clogged arteries, the lungs might illustrate reduced capacity and potential for respiratory issues, the liver could display fatty deposits and scarring, the kidneys could show signs of damage, and the joints could exhibit signs of osteoarthritis.
The overall picture should visually communicate the cumulative negative impact of obesity on multiple organ systems over time, highlighting the importance of prevention and management.
Ultimate Conclusion
So, we’ve journeyed through the landscape of obesity health issues, from its prevalence and physical consequences to its mental health ramifications and treatment options. Remember, managing weight is a holistic endeavor, requiring a multifaceted approach that addresses both physical and emotional well-being. By understanding the complexities involved, we can better support individuals and communities in their pursuit of a healthier lifestyle.
Let’s work together to build a healthier future!
Frequently Asked Questions
What are some common misconceptions about obesity?
Many believe obesity is simply a matter of willpower. However, it’s a complex condition influenced by genetics, environment, and societal factors. Another misconception is that all weight loss methods are created equal – finding a sustainable approach tailored to individual needs is crucial.
Can obesity be reversed?
While complete reversal might be challenging, significant weight loss is achievable through lifestyle changes and medical interventions. The key is sustained commitment to healthy habits and seeking professional support when needed.
What role does stress play in obesity?
Stress can lead to increased cortisol levels, promoting fat storage, particularly around the abdomen. Managing stress through techniques like exercise, mindfulness, and adequate sleep is essential for weight management.
Are there any natural ways to manage obesity?
Absolutely! A balanced diet rich in fruits, vegetables, and whole grains, combined with regular exercise, is fundamental. Mindful eating practices and stress reduction techniques can also significantly contribute to weight management.