Ever wondered how we can tackle the global obesity epidemic? The answer lies partly in effective health education. This isn’t just about lectures and pamphlets; it’s about creating lasting lifestyle changes through engaging programs tailored to different ages and communities. We’ll explore the science behind obesity, examine successful interventions, and discover how even pharmacists play a vital role in this fight for better health.
From understanding the complex interplay of genetics, environment, and behavior to designing effective campaigns and measuring their impact, we’ll delve into the strategies that truly make a difference. We’ll also uncover practical tools and resources you can use to improve your own health and the health of those around you, making healthier choices more accessible and appealing.
Defining Health Education in Obesity Prevention

Health education plays a crucial role in preventing obesity by empowering individuals with the knowledge, skills, and motivation to adopt and maintain healthy lifestyles. Effective programs move beyond simply providing information; they foster behavioral change through interactive strategies and community support. The core principles of successful interventions are built upon understanding individual needs and tailoring approaches accordingly.
Core Principles of Effective Health Education Programs Targeting Obesity
Effective health education programs for obesity prevention are built on several key principles. These programs prioritize creating a supportive environment that encourages healthy choices and provides the necessary tools for sustained behavior change. They also focus on long-term lifestyle modifications rather than short-term fixes. A multi-faceted approach, incorporating various educational strategies and community involvement, is essential. Finally, regular evaluation and adjustment are vital to ensure the program’s effectiveness and adapt to evolving community needs.
Successful Health Education Interventions for Different Age Groups
Tailoring interventions to specific age groups is vital for effectiveness. For children, programs might focus on fun, interactive activities promoting physical activity and healthy eating, like incorporating games and interactive lessons in school settings. Examples include school-based programs that integrate nutrition education into the curriculum and offer healthy snacks. For adolescents, interventions might address peer pressure and media influence on body image, employing strategies such as social media campaigns promoting positive body image and healthy lifestyle choices.
Adult programs could emphasize stress management techniques, cooking classes focusing on healthy recipes, and workplace wellness initiatives to encourage physical activity during work hours. Successful interventions often use a combination of educational materials, community-based activities, and individual counseling.
The Role of Community Engagement in Obesity Prevention Health Education Initiatives
Community engagement is paramount in successful obesity prevention efforts. It involves actively collaborating with community members, leaders, and organizations to create a supportive environment that promotes healthy choices. This can involve partnering with local businesses to offer healthier food options, collaborating with community centers to provide fitness classes, and working with faith-based organizations to promote healthy lifestyles within their communities.
Successful initiatives often involve community-based participatory research, ensuring that programs are culturally relevant and meet the specific needs of the target population. This collaborative approach fosters a sense of ownership and sustainability, ensuring long-term impact.
A Health Education Campaign Focusing on Healthy Eating Habits for a Specific Community
Let’s consider a campaign targeting a low-income urban community with limited access to healthy food options. The campaign, titled “Nourishing Our Neighborhood,” could involve several key components. First, a series of cooking demonstrations and workshops teaching participants how to prepare affordable, nutritious meals using readily available ingredients. Second, partnerships with local grocery stores to offer discounts on healthy foods and create designated “healthy corner” displays featuring affordable fruits, vegetables, and whole grains.
Third, a community garden initiative, empowering residents to grow their produce, fostering a sense of community and providing access to fresh, healthy food. Fourth, a social media campaign using relatable images and videos to showcase the benefits of healthy eating and recipes that fit within the community’s budget. Finally, regular community events promoting healthy eating and physical activity would reinforce the campaign’s message and foster a supportive environment.
The campaign’s success would be measured by changes in dietary habits, community engagement levels, and increased access to healthy food options. This multi-pronged approach addresses multiple barriers to healthy eating, improving the community’s overall well-being.
Understanding the Causes and Consequences of Obesity
Obesity is a complex health issue stemming from an intricate interplay of genetic predisposition, environmental influences, and behavioral choices. Understanding these factors is crucial for developing effective prevention and treatment strategies. This section will explore the root causes of obesity and its significant short-term and long-term health implications. We will also examine various approaches to managing and treating obesity.
Genetic Factors in Obesity
Genes play a significant role in determining an individual’s susceptibility to weight gain. Certain genes influence metabolism, appetite regulation, and fat storage. While genetics don’t dictate obesity definitively, they can create a predisposition, making some individuals more prone to weight gain than others even with similar lifestyles. For example, research has identified specific genes linked to increased appetite or decreased energy expenditure.
These genetic predispositions, however, do not eliminate the impact of environmental and behavioral factors.
Environmental Factors Contributing to Obesity
Our surroundings significantly impact our weight. Easy access to highly palatable, energy-dense foods, coupled with a decrease in physical activity, creates an obesogenic environment. Factors such as food marketing targeting children, the prevalence of fast-food restaurants, and the lack of safe spaces for physical activity in many communities all contribute to increased obesity rates. Furthermore, socioeconomic factors like food insecurity and lack of access to healthy food options disproportionately affect certain populations.
Behavioral Factors and Obesity
Individual behaviors, such as dietary habits and physical activity levels, are major determinants of weight. Consuming excessive calories, particularly from processed foods high in sugar and unhealthy fats, contributes to weight gain. Conversely, insufficient physical activity leads to a calorie surplus, promoting fat accumulation. Sedentary lifestyles, prevalent in modern society due to increased screen time and reliance on cars, exacerbate this problem.
Stress and poor sleep habits also influence appetite and metabolism, potentially leading to weight gain.
Short-Term and Long-Term Health Consequences of Obesity
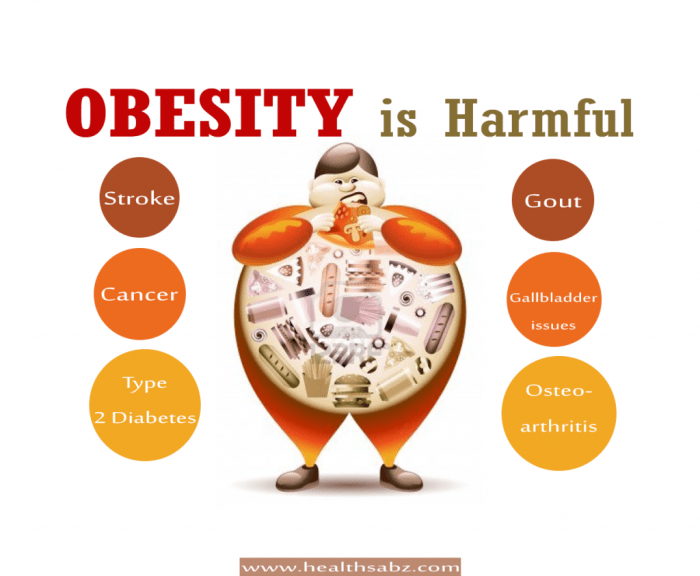
Obesity is associated with a multitude of short-term and long-term health problems. Short-term consequences can include sleep apnea, joint pain, and decreased physical fitness. More serious long-term consequences include type 2 diabetes, cardiovascular disease (including heart attacks and strokes), certain types of cancer, non-alcoholic fatty liver disease, and osteoarthritis. The severity of these complications is often directly related to the degree of obesity.
For example, individuals with a higher BMI are at significantly increased risk of developing type 2 diabetes.
Obesity Treatment Approaches
Various approaches exist for managing and treating obesity, often involving a combination of strategies. These include lifestyle modifications such as dietary changes (balanced nutrition with reduced calorie intake), increased physical activity, and behavioral therapy to address eating habits and emotional responses to food. Pharmacological interventions, such as appetite suppressants or medications that enhance satiety, may be considered in certain cases.
Bariatric surgery, a more invasive option, is reserved for individuals with severe obesity who haven’t responded to other treatments. The most effective approach is often personalized to suit an individual’s needs and circumstances.
Risk Factors and Their Impact on Obesity Development
| Factor | Description | Impact | Intervention |
|---|---|---|---|
| Genetics | Inherited traits influencing metabolism, appetite, and fat storage. | Increased predisposition to weight gain. | Genetic counseling (in some cases), focus on lifestyle modifications to mitigate genetic risk. |
| Unhealthy Diet | High consumption of processed foods, sugary drinks, and unhealthy fats. | Excess calorie intake leading to weight gain. | Dietary education, adopting a balanced diet, portion control. |
| Lack of Physical Activity | Sedentary lifestyle with insufficient exercise. | Reduced calorie expenditure, promoting weight gain. | Increasing physical activity through regular exercise, incorporating movement into daily routine. |
| Socioeconomic Factors | Limited access to healthy food, safe exercise spaces, and resources. | Increased reliance on inexpensive, less healthy options; reduced opportunities for physical activity. | Policy changes to improve access to healthy food and safe exercise environments, community-based programs. |
Strategies for Promoting Healthy Lifestyles
Combating obesity requires a multifaceted approach that empowers individuals to adopt and maintain healthy lifestyles. This involves promoting physical activity, improving dietary habits, and providing readily accessible resources and support. The strategies Artikeld below focus on evidence-based interventions tailored to diverse populations.
Promoting Physical Activity Across Populations
Effective strategies for increasing physical activity vary depending on the target population. For children and adolescents, school-based programs incorporating physical education and active breaks are crucial. These programs should emphasize fun and engagement, rather than focusing solely on competition. For adults, workplace wellness programs, community-based initiatives (such as walking groups or fitness classes), and accessible public parks and recreational facilities are effective.
Older adults benefit from low-impact exercises like water aerobics or chair yoga, tailored to their physical capabilities and potential health concerns. Creating supportive social environments, where physical activity is normalized and encouraged, is also vital across all age groups. For example, promoting family walks or cycling trips can foster a positive association with physical activity.
Improving Dietary Habits and Reducing Unhealthy Food Consumption
Improving dietary habits necessitates a shift towards whole, unprocessed foods and a reduction in sugary drinks and processed snacks. Educational campaigns that focus on nutrition literacy, emphasizing portion control and mindful eating, are effective. Making healthy food choices more accessible and affordable is crucial, particularly in low-income communities. This includes supporting farmers’ markets, promoting healthy food options in schools and workplaces, and implementing policies that encourage healthy food production and distribution.
Furthermore, strategies like front-of-package labeling, restricting advertising of unhealthy foods to children, and implementing sugar taxes can help to reduce the consumption of unhealthy foods. For instance, Chile’s implementation of warning labels on packaged foods has demonstrably influenced consumer choices.
Resources for Supporting Healthy Lifestyle Changes
Access to reliable information and support is vital for successful lifestyle changes. Here are some key resources:
- Registered Dietitians and Nutritionists: These professionals can provide personalized dietary guidance and support.
- Certified Personal Trainers: These professionals can design safe and effective exercise programs.
- Online Resources: Reputable websites such as the CDC and NIH offer evidence-based information on healthy eating and physical activity.
- Community Centers and Fitness Facilities: These locations offer classes, programs, and equipment to support healthy living.
- Support Groups: Connecting with others who share similar goals can provide motivation and accountability.
Developing Personalized Nutrition Plans
A personalized nutrition plan should consider individual factors like age, sex, activity level, dietary preferences, and any existing health conditions. It’s crucial to start with a balanced approach, emphasizing whole grains, fruits, vegetables, lean protein, and healthy fats. Portion control is key; using smaller plates and measuring food can help regulate intake. Tracking food intake using a food diary or app can enhance awareness of eating habits.
Regular consultations with a registered dietitian can ensure the plan is effective, safe, and sustainable. For example, a plan for a highly active individual will differ significantly from one designed for a sedentary individual, reflecting the varying energy requirements. Furthermore, accommodating personal preferences and cultural factors within the plan is vital for long-term adherence. For example, substituting certain foods with culturally similar alternatives can enhance compliance.
The Role of the Pharmacy in Obesity Prevention
Pharmacists are uniquely positioned to play a vital role in obesity prevention and management. Their accessibility, expertise in medication management, and patient interaction opportunities create a powerful platform for promoting healthy lifestyles and improving patient outcomes. Beyond dispensing prescriptions, pharmacists can actively contribute to reducing the burden of obesity through various interventions.
Pharmacist Counseling and Education on Obesity Prevention
Pharmacists can provide crucial counseling and education to patients regarding obesity prevention and management. This includes discussing the risks associated with obesity, such as type 2 diabetes, heart disease, and certain cancers. They can offer personalized advice based on individual patient needs and preferences, considering factors like age, lifestyle, and existing health conditions. Effective communication techniques, including motivational interviewing, can encourage patients to adopt healthier habits.
For example, a pharmacist could explain how even small changes, like reducing sugary drinks or increasing daily steps, can significantly impact overall health.
Pharmacy-Based Interventions for Medication Adherence
Many individuals with obesity-related conditions, such as diabetes or hypertension, require medication adherence for effective management. Pharmacists play a critical role in improving medication adherence through various strategies. These include providing clear and concise medication instructions, using medication organizers or blister packs to simplify medication regimens, and proactively contacting patients to address any concerns or barriers to adherence. For instance, a pharmacist could implement a system of regular follow-up calls to patients prescribed metformin for type 2 diabetes, addressing potential side effects and reinforcing the importance of consistent medication use.
Furthermore, pharmacists can actively participate in medication reconciliation, ensuring patients are on the most appropriate and effective medications for their conditions.
Promoting Healthy Lifestyle Choices and Referrals
Pharmacists can actively promote healthy lifestyle choices by providing information and resources on healthy eating, regular physical activity, and stress management techniques. They can assess patients’ lifestyle habits during consultations and offer tailored recommendations. This could involve suggesting dietary changes, recommending suitable exercise programs, or referring patients to registered dietitians, certified personal trainers, or mental health professionals for additional support.
For example, a pharmacist could provide patients with brochures on healthy meal planning or connect them with local community programs offering affordable fitness classes. They can also screen patients for depression and anxiety, conditions often linked to obesity, and facilitate referrals to appropriate mental health services.
A Pharmacist’s Pamphlet on Obesity Prevention and Management
Understanding Obesity: Obesity is a complex condition characterized by excessive accumulation of body fat, increasing the risk of various health problems. It’s crucial to adopt a holistic approach to prevention and management.
Healthy Eating: Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Limit processed foods, sugary drinks, and unhealthy fats. Portion control is key! Consider consulting a registered dietitian for personalized dietary guidance.
Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities twice a week. Find activities you enjoy and make them a regular part of your routine.
Available Resources: Your pharmacist can provide you with information on local support groups, weight management programs, and other relevant resources to assist you in your journey towards a healthier lifestyle. Don’t hesitate to ask for help! We are here to support you.
Measuring the Effectiveness of Health Education Programs

Evaluating the success of health education programs aimed at combating obesity requires a robust and multifaceted approach. We need to move beyond simply counting participants and delve into the actual impact on individuals’ health and the broader community. This involves carefully designed methods to measure changes in behaviors, health outcomes, and ultimately, obesity prevalence.Effective measurement is crucial for demonstrating program value, informing future program improvements, and justifying continued funding.
It’s about showing the return on investment, both in terms of healthier individuals and a healthier society.
Methods for Evaluating Program Impact
Assessing the effectiveness of obesity prevention programs necessitates a variety of evaluation methods, combining quantitative and qualitative approaches for a comprehensive understanding. Quantitative methods focus on numerical data, while qualitative methods explore the experiences and perspectives of participants. This integrated approach allows for a richer and more nuanced understanding of the program’s impact.Quantitative methods often involve comparing pre- and post-intervention data on key indicators like BMI, waist circumference, dietary habits, and physical activity levels.
Statistical analysis then helps determine whether significant changes have occurred. Qualitative methods, such as focus groups and interviews, can provide valuable insights into the reasons behind observed changes or lack thereof, helping to refine program strategies.
Key Indicators for Assessing Effectiveness
Several key indicators are crucial for a comprehensive assessment of obesity prevention interventions. These indicators provide a clear picture of the program’s success in achieving its objectives. These indicators are not mutually exclusive and often complement each other.
- Changes in BMI and Waist Circumference: These are fundamental measures of obesity, providing a direct assessment of weight changes.
- Improvements in Dietary Habits: Tracking changes in fruit and vegetable consumption, sugar-sweetened beverage intake, and overall dietary quality provides insights into behavioral modifications.
- Increased Physical Activity Levels: Measuring changes in the frequency, intensity, and duration of physical activity provides a crucial indicator of lifestyle improvements.
- Enhanced Knowledge and Self-Efficacy: Assessing participants’ understanding of healthy lifestyles and their confidence in maintaining healthy behaviors is essential for long-term success.
- Changes in Health Outcomes: Monitoring changes in blood pressure, cholesterol levels, and other relevant health markers demonstrates the program’s impact on overall health.
Data Collection Tools and Analysis Techniques
The choice of data collection tools and analysis techniques depends heavily on the specific program objectives and target population. However, some common approaches are widely used.
- Surveys and Questionnaires: These are efficient tools for collecting self-reported data on dietary habits, physical activity, and knowledge levels. Validated questionnaires are preferred to ensure reliability and validity.
- Biometric Measurements: BMI, waist circumference, blood pressure, and cholesterol levels can be measured directly using standard procedures. This provides objective data on physiological changes.
- Physical Activity Monitors: Wearable devices or accelerometers provide objective data on physical activity levels, providing a more accurate measure than self-report alone.
- Focus Groups and Interviews: These qualitative methods provide valuable insights into participants’ experiences and perceptions of the program, informing future program improvements.
- Statistical Analysis: Techniques like t-tests, ANOVA, and regression analysis are used to analyze quantitative data and determine the statistical significance of observed changes.
Illustrative Example of Measuring Program Success
The following table illustrates how to measure the success of an obesity prevention program using various metrics, measurement methods, targets, and evaluation criteria.
| Metric | Measurement Method | Target | Evaluation |
|---|---|---|---|
| BMI | Pre- and post-intervention measurements | Average reduction of 2 BMI points | Compare pre- and post-intervention means using a paired t-test. Assess the percentage of participants achieving the target reduction. |
| Fruit and Vegetable Consumption | Food frequency questionnaire | Increase daily servings from 2 to 4 | Analyze changes in average daily servings using a paired t-test. |
| Physical Activity (minutes/week) | Self-reported questionnaire and accelerometers | Increase from 150 to 300 minutes/week | Compare pre- and post-intervention means using a paired t-test. Assess the percentage of participants achieving the target increase. |
| Knowledge of Healthy Eating | Pre- and post-intervention knowledge test | Increase in correct answers by 20% | Compare pre- and post-intervention scores using a paired t-test. |
| Program Satisfaction | Post-intervention survey | Average satisfaction rating of 4 out of 5 | Calculate the average satisfaction rating and assess the percentage of participants reporting high satisfaction. |
Final Summary
Combating obesity requires a multifaceted approach, and health education forms the bedrock of sustainable change. By understanding the root causes, implementing evidence-based strategies, and continuously evaluating our efforts, we can empower individuals and communities to make healthier choices. This isn’t just about weight loss; it’s about improving overall well-being and building a healthier future, one informed choice at a time.
Let’s work together to create a world where healthy living is the norm, not the exception!
FAQ Compilation
What are some common misconceptions about obesity?
Many believe obesity is simply a matter of willpower. However, it’s a complex issue influenced by genetics, environment, and societal factors. Another misconception is that all diets work equally well; personalized approaches are key.
How can I get involved in promoting health education on obesity in my community?
Volunteer at local health organizations, participate in community events focused on health and wellness, or even start a small initiative in your neighborhood promoting healthy eating and physical activity.
Are there specific health education programs designed for children?
Absolutely! Many programs focus on teaching children about healthy eating habits and the importance of physical activity through fun, interactive activities and age-appropriate lessons.
What role does technology play in obesity prevention health education?
Technology plays a huge role! Apps for tracking fitness, nutrition, and even providing personalized health coaching are readily available. Online resources and social media can also be effective tools for spreading awareness and sharing information.